Abstract

Introduction: Treatment of relapsed or refractory classical Hodgkin lymphoma (R/R cHL) in patients considered ineligible for stem cell transplant (SCT) in the United States (US) has evolved since 2011. It is important to understand the current treatment landscape and the outcomes associated with current standards of care as new treatment options have been introduced. This analysis provides recent real-world evidence on patient characteristics, treatment patterns, and outcomes in R/R cHL patients in the US who are initially considered ineligible for SCT and are treated with or without brentuximab vedotin (BV).
Methods: Hematologists and oncologists (N=205) from the US retrospectively identified patients diagnosed with R/R cHL who received at least two lines of therapy and received their most recent line of therapy between January 2014 and May 2018. The physicians were responsible for abstracting data and completing response forms for variables of interest. The current analysis focused on patients who were considered ineligible for SCT by their physician: descriptive statistics on patient demographics/clinical characteristics, treatment patterns, and outcomes by line of therapy; bivariate analyses (chi-square) comparing treatment modalities by line of therapy.
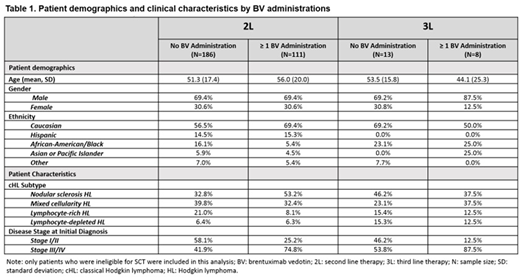
Results: Physicians retrospectively identified 297 patients that they considered ineligible for SCT. Mean (SD) age at initial cHL diagnosis was 53.0 (18.5), most patients were male (69.4%) and Caucasian (61.3%). The most common cHL subtype at diagnosis was nodular sclerosis HL (40.4%), and patients had either Stage I/II (45.8%) or Stage III/IV (54.2%) cHL at initial diagnosis. Median follow-up time for the cohort included here was 15.96 months from initiation of 1L treatment.
The majority of the cohort (N = 297) received systemic therapy alone (84.5%) compared to those who received systemic therapy in combination with radiation therapy (RT) (15.5%) in 1L. 1L systemic regimens included regimens that contained ABVD alone or ABVD in combination with other regimens (69.4%). Of those who used ABVD alone or in combination with another regimen (N = 206), 24.8% used a PET adapted approach and deescalated to AVD (N = 51) and 11% escalated to be BEACOPP (N = 18). Other systemic regimens included AVD (10.1%), BEACOPP (7.4%) and ICE (5.7 %). The majority of patients achieved a complete response (CR) or partial remission (PR) after 1L therapy (41.4%, 38% respectively) while 34.1% (N = 61) failed to achieve remission or progressed while on therapy.
The most common systemic regimens in 2L (N = 293) were BV monotherapy or in combination with bendamustine (34.6%), salvage regimens [including ICE, DHAP, ESHAP or gemcitabine based combinations] (33%), re-challenge with a previous 1L regimen (19.5%), and PD-1 inhibitors (10.8%). Very few patients received systemic therapy in combination with RT (6.7%) in 2L.The most common systemic regimens used in 3L (N = 21) for the selected cohort of patients not eligible for SCT were BV monotherapy (28.6%) and PD-1 inhibitors (33.3%). Median (range) number of cycles in 2L and 3L was four (1-18) and two (1-14), respectively. Treatment outcomes were variable for patients in 2L and 3L. In 2L, 27.6% achieved a CR, 25.6% achieved a PR, while 24.2% and 15.8% were refractory or progressed on treatment. There were no CRs reported in 3L (N = 21). 26 patients died in 2L and 3L combined.
Conclusion/Summary: Given the rapid evolution of therapies used to treat R/R cHL, these findings fill a crucial data gap in real-world evidence on patient characteristics, treatment patterns, and outcomes of patients deemed SCT ineligible in the US.
Feliciano:Seattle Genetics: Employment. Way:Kantar Health: Employment; Seattle Genetics: Research Funding. Engley:Seattle Genetics: Employment. Ghosh:Juno: Consultancy, Research Funding; SGN: Consultancy, Research Funding, Speakers Bureau; PCYC: Consultancy, Research Funding, Speakers Bureau; Celgene: Consultancy; Spectrum: Consultancy; Gilead: Consultancy, Speakers Bureau; Pharmacyclics, an Abbvie Company: Consultancy, Research Funding, Speakers Bureau; Genentech: Research Funding; F. Hoffman-La Roche Ltd: Research Funding; Abbvie: Consultancy, Speakers Bureau; Forty seven Inc: Research Funding; TG Therapeutics: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal